I want you to picture a dumpster. A bad one, full of rotting fast food, like a McDonalds-parking-lot-at-3am dumpster. One that no one bothers to lock or protect from animals because even the racoons will stay away from the fermenting, rancid waste.
Got a mental picture? Now place that dumpster aboard a Viking funeral of a ship, ablaze, sailing toward an enormous waterfall with nothing but jagged rocks below.
Welcome to the field of emergency medicine! We hope you enjoy your brief stay before you are forced by scarcity to seek alternative employment.
In case you think this is alarmist: one of the major emergency medicine professional societies, ACEP, recently published a bombshell report that predicts a frank oversupply of emergency physicians by 2030, to the tune of 7,000-10,000 bodies. You should be alarmed!
This report was published in June in one of the top EM journals, Annals of Emergency Medicine (resisting the urge to make a joke about anal has always been difficult). As is customary for highly-trained medical professionals, we had a couple of roundtable discussions about it, recorded some podcast episodes, and then promptly went back to burying our heads in the sand and pretending that the problem does not exist.
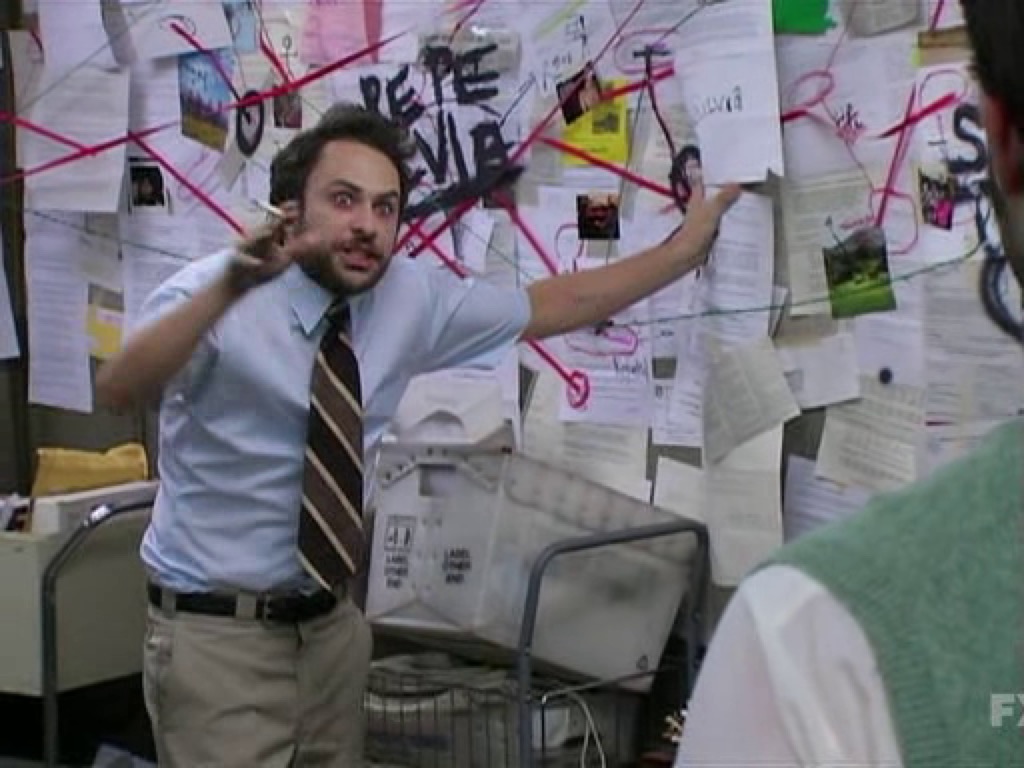
What we really should be doing, professionally speaking, is LOSING OUR SHIT. Training to completion in emergency medicine requires at least seven to eight years of post-bachelors training. Most trainees make it through med school with an astounding loan burden (up to half a million dollars is not unusual), then must defer real income or repayments while they complete residency. And now, as fresh grads, we’ve learned that the security of gainful employment is closer to wishful thinking.
How did we end up here, craning our heads around and exclaiming, “what the FUCK!?” The answer is complicated enough to justify a dissertation, but it basically boils down to two interlocking factors that emergency physicians have willfully ignored for the entire forty-year existence of the specialty.
(You would think that highly trained, intelligent medical professionals like ourselves would have seen the hamfisted intrusion of pure unbridled capitalism into the doctor-patient relationship, but you would be wrong. At heart we are a bunch of nerds who willfully ignored any discussions of finance for years, because if we listened we would have understood that going into medicine was a horrendously risky financial/life decision and chosen a smarter career path.)
The next 500 words or so are not very funny. Please feel free to skip if you are not a blood relative or are otherwise not deeply invested in my well-being.
Anyway. First, ER doctors used to belong to groups that would staff one or sometimes a few area emergency departments. They had equity in these small groups and made decisions together. Over time, corporations backed by private equity – banks and hedge funds, mostly – purchased pretty much all of these groups and rolled them into progressively larger companies called contract management groups, or CMGs. In essence, emergency physicians gave up their autonomy and ownership and became punchcard operators in exchange for a slightly higher payday. At the same time the market was consolidating, EM exploded in popularity and hospitals began opening ER residencies as fast as they could. In many cases, these residencies opened at hospitals where CMGs owned the ER contract, which should at least make you wonder if these companies were intentionally advocating for more residency programs to increase their workforce supply.
I advise you to not think about that too hard. It is a small step from that line of questioning to full blown conspiracy theory.
Second, nurse practitioners and physician assistants – often lumped together as “midlevels,” “advanced practice providers,” and probably some other euphemisms – entered the ER. Initially, they required supervision by an ER doctor, but in most states that requirement has steadily eroded away. (If you go to an ER and you’re not actively dying, the chances you are seen by a PA or NP is somewhere between 20-40%.) Training to become a nurse practitioner or a physician assistant is far less time-consuming and far cheaper than getting an MD/DO and completing residency, so of course many people are taking advantage of this route. Numbers of these providers are exploding.
The discussion of whether this is a good thing or not is beyond the scope of this post, which is code for, “I do not want a midlevel-sized army of enraged health professionals or pseudoprofessionals demolishing my inbox with emails full of all-caps internet hate.” These providers are here to stay, not the least of which is because an NP salary is about one-third that of an emergency physician. If you’re a CMG, it’s a no-brainer: instead of staffing six ER doctor shifts a day, cut that down to two and fill in twice as many NPs or PA. You save money. Do patients notice? Is the delivery of healthcare affected?
The better question is, who cares?
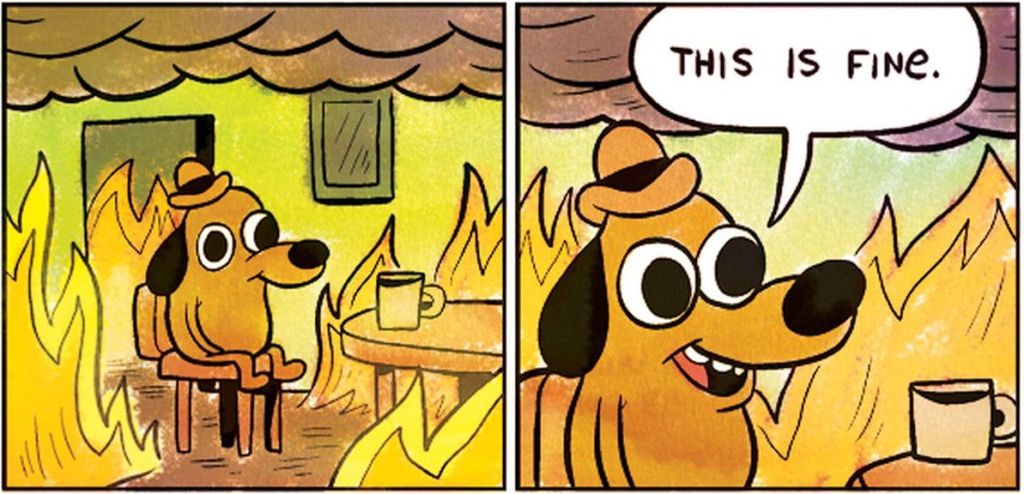
Despite these problems, there remain some ER doctors who I have dubbed (as of right now) the This Is Finers: calming presences who soothingly intimate that we will all be okay, that the jobs will still be there in perpetuity, and that corporate America would never interfere in the sanctity of the patient-doctor relationship.
The This Is Finers are almost universally elder statesmen of the field. I mean no offense: in medicine we stand on the shoulders of those who came before us, and many of the TIF’ers are respected wise people with tremendously successful careers in EM. Of course, this is exactly the problem! The TIFers are the most senior professionals we have. No one is going to fire them. Most of them will retire before the job crunch hits.
So their perspective is basically useless to new graduates or prospective EM applicants. The rest of us are too busy scrambling to meet the demands of our corporate masters to raise the alarm: as I write this, I’m typing an order for a weight-based bag of saline and some antibiotics for a patient who I am quite confident is having a panic attack, but who triggered an electronically generated alert for sepsis. If I do not administer an unnecessary dose of vancomycin in the next five minutes, I will be demerited like a disobedient schoolboy and replaced by someone better at wringing compensation dollars out of Medicare.
(This is a slight exaggeration. I used ceftriaxone like other reasonable people.)
(Also, I’m obviously not blogging on shift. That would require break time.)
I certainly don’t have a solution for these problems. That’s for smarter people with more determination than me, and the only thing I’m currently motivated by is getting a full night of sleep and some chocolate. But if anyone reading this is considering a career in EM… think again.


Very funny, but you’re risking life and limb in that paragraph about nurses.
Love the TIFs! Also the graph in parentheses.
When you write humor, I know you’re still sane.
You know EM providers are doing fellowships, right? Lots of them are going into CCM, and more will follow. EM is not necessarily the end of the road.
And you should probably learn a little more about the differences between PAs and NPs before you lump them together under the perjorative “midlevel” (for example, did you know PAs have to do more than twice the number of clinical hours as NPs before graduating?) I’ve worked with lots of PAs that I would gladly trust myself or my family member to in a life-or-death emergency.
@noblecountyscholarsfund – indeed, I do know that. I don’t think ‘midlevel’ is perjorative, it’s just easier/shorter to write that or APP instead of “NPs and PAs, who have different training and certifications and licensing boards but fill largely identical niches in the emergency department.” I also know and work with great NPs and PAs and have nothing against them.
As for fellowship, yes I am aware of this considering I’m currently a medical toxicology fellow, which I chose to do because the writing is clearly on the wall. I would suggest to you that if a doctor must specialize out of their field to survive, maybe the field is not doing well. And as it sounds like you know, fellowship spots are also quite limited and the vast majority of EM grads will not follow up their already superlong training with additional deferred income by doing fellowship.
As an about to be new grad nurse sucking up for my 6mos-1year of bedside dayshift hell…. I am finally commenting as a silent reader. Your blog is phenomenal and hilarious. There’s no way your midlevel commentary is pejorative (spelling bee word right there) in any sense. Corporations gonna corporate- the bigger they get the worse the front line people’s work lives get too (a slight interjection for the fact military front line, gets lifelong healthcare and a free degree dashed in with potential death. I get….. a rock, some pizza, and words of sincere gratitude by our multi-millionaire CEO. Sprinkle in assault (not a felony against a HCW in most states), verbal abuse and…. 60% charting and you’ve got: yay! bedside!).
My fav line: more importantly- who cares?
Exactly. I tell my fam- don’t get sick, yay! Otherwise to all my future pts- watch out because we all start in July and we all learn things by people dying first while learning HA! Go medicine. 😀
I am getting out of bedside then doing local travel or prn work then clinic for me bc Imma cog it up where I’m much less likely to screw up the singular back I’ve been given for the duration of my life.
Party goer that’s fam med resident grad in July was telling me how EM residents couldn’t get jobs this last yr bc corp was like yes one ER dr cheaper we shall just staff one. I presume in the next 5-10 years a new nursing cert will exist between LPN and RN and it will specialize out into 1 nurse does all wounds, 1 nurse does all IV meds etc etc like the automatons we are meant to be.
Keep writing. Hope your dog is doing well.
LOST it at the rock comment. So true. We got pizza once and a nice sign saying we were heroes.