I wrote before about how emergency medicine is, in my opinion, a dying field. Maybe it’s already dead. Emergency departments and their physicians have lost the war on multiple fronts: declining reimbursement from payers, declining interest from medical students, pay cuts, increasing liability, encroachment from midlevel providers, and a lack of offramps. To spare your attention span, here are some bullet points – facts, not opinions.
- Emergency department reimbursement overall took a 3% pay cut in 2024, despite record volumes essentially everywhere
- Emergency medicine applications peaked before COVID and took an absolute NOSEDIVE afterward. The EM match in 2023 was a total dumpster fire of vacant residency positions that ended up getting filled through a process called SOAP, which is where people who wanted to go into a different field and failed can instead scramble for the leftover breadcrumbs in other fields. What was once one of the more competitive medical fields for residency is now at the bottom.
- The numbers of applications has rebounded, but the candidates applying for these are now disproportionately international medical graduates (IMGs). Nothing against IMGs, but the best and brightest are no longer seeking training in this field. Because they are the best and brightest.
- Emergency medicine physician compensation, when adjusted for inflation is down TWENTY PERCENT in the last 5 years! An EM physician in 2012 was making almost the exact same salary as an EM physician thirteen years later. In the linked report, emergency medicine was the only field to see a drop in inflation-adjusted income. The only one.
- Despite the above, emergency departments are busier than ever, seeing year-over-year record volumes and suffering longer and longer wait times. This is occurring alongside a backdrop of a massive nursing shortage that is projected to worsen in the next five years.
The problems within the house of emergency medicine are innumerable – you could probably write a whole book – but one unifying feature so far is the near-total absence of any kind of ability to stand up for ourselves. We are huge wimps who roll over and take whatever we are given, like Otis begging for table scraps.
Why is this? EM is a somewhat unique field within medicine: we don’t have our own patients. This is freeing but also a terrible handicap – we carry no independent value to an employer.
An EM doctor in Utah can pick up a Virginia medical license and start working in a Richmond ER as fast as the hospital’s sloth-like credentialing department can move. Many of us work locums: we drive and fly around to different emergency departments all over the States, chasing the highest rate we can find. I know a guy that lives in L.A. and flies to rural Oklahoma once a month to work seven 12-hour shifts in a row, because he is a sociopath with mouths to feed, and, I guess, Delta status to maintain.
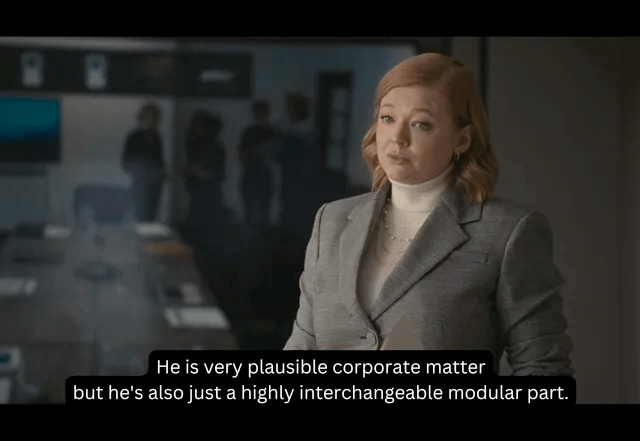
This sounds great in some ways, but it means EM doctors are pure mercenaries. We are, in the words of Shiv Roy, highly interchangeable modular parts. We are highly trained experts, to be sure, but we are no more unique than a robot arm at a Nissan factory cranking out Sentras. Plug us in anywhere and we’ll do the exact same job as the next guy.
Is there variation in our skill and efficiency and thinking? Sure. Are there good and bad ER doctors? Absolutely. Does this matter to a hospital? No. Not even a little bit.
There is, in fact, a way to improve our lot: organizing. Emergency medicine physician need to unionize, and we need to unionize on a gigantic, national scale. Fuck it.
It is bananas that we ER docs go through twelve years of post-secondary training, acquire a broad and specialized skill set, and then accept the same negotiating power as an Amazon warehouse employee. The baristas at the hospital Starbucks are better organized than we are. It is wild that we are told, year after year, that we should do more with less, get paid less, and work harder… but what’s crazier is that we just accept it!
We only have ourselves to blame: for drinking the medical school Kool-Aid (we had mandatory professionalism classes and were taught that being a physician is a “Higher Calling,” which is hilariously untrue in the hellscape that is the ER); for accepting more and more responsibility and liability without asking for help or appropriate pay; for not standing up for ourselves when hospital administration adds on more dumb metrics to hit each quarter, as if the ED is a truck stop Carl’s Jr. franchise with struggling burger-to-car numbers.
An example of a partial job listing I saw posted yesterday for a major East Coast city hospital:
- “$190+/hr” day shifts and $200/hr night shifts
- “$40/hr of world-class benefits”
- 10- and 12-hour shifts
There’s a lot wrong with this posting – for example, it omits how busy the shifts are, which means they are toxic dumpster fires full of nightmares and sadness – but I think just the top line finding of $190 an hour for supposed expert-level medical care is awful enough.
For reference, my buddy’s pool guy comes once a week for 10 minutes to clean the filters and earns $200 a month for less than an hour of total work. My other friend is a corporate finance lawyer, sits behind a desk all day, and charges $800/hour. Also, she gets raises and end-of-year bonuses, and sometimes free donuts.
I also get free donuts sometimes, but only when Rhoda is charge nurse. ❤
Anyway. The only reason jobs like this actual, real-life shitpost exist is because the EM job market is trash and people end up desperate and taking whatever scraps are offered.
Organizing momentum has, so far, been nonexistent. A few small democratic groups here and there have formed unions, but what we really need is a large, regional- or national-sized effort that gives us actual leverage in numbers. Right now, if your small group unionizes, the hospital can just tell you to piss off and replace your group with one of the big mercenary staffers: USACS, Vituity, TeamHealth, etc.
This is the most common scenario response to a union threat. It is also the worst-case scenario.
These large corporate organizations staff hundreds of ERs across the country each and have thousands of individual ER doctors on their rosters. They offer an economy of scale that the smaller groups can’t match, so they squeeze out these groups. They aim to command a large market share in a geographic area, and then undercut salaries and benefits because there’s no other good option.
We need unions that represent all TeamHealth employees, not just 12 doctors in a tiny group. We need a union that can tell an HCA hospital network, “either you negotiate with us or you’re going to be locked out of the entire professional labor pool.” We need to swallow our pride and brainwashing – the brainwashing that says we physicians are leaders of men and women and we are above such peasantry – and recognize that only by collective action can we meaningfully improve what is rapidly becoming the worst physician job in healthcare.
Or we just run out the clock until AI takes over and hospital ER’s just become the autodoc box from the bad comedy/unintentional documentary Idiocracy:

( All of this explains why I’m so saddened by the current cr
Ok. So. I wonder if you can divert your vision toward policy wonks. There is so much good material here, and also in your last one. You identify the issues, and make suggestions, which is exactly what needs to be published. But where? What are the publications geared toward ER medicine. I think you should start to publish these. Make them work. Make people rethink. Making change requires a loud voice which is what you have. Use your expertise and reflection to do something active. MAKE CHANGE.