I wrote before about how emergency medicine is, in my opinion, a dying field. Maybe it’s already dead. Emergency departments and their physicians have lost the war on multiple fronts: declining reimbursement from payers, declining interest from medical students, pay cuts, increasing liability, encroachment from midlevel providers, and a lack of offramps. To spare your attention span, here are some bullet points – facts, not opinions.
Continue readingMedicine
A Bird in the Hand
I will preface this story with a disclaimer: I am not exaggerating the following.
On one short-handed urgent care shift right before Christmas, wait times to see the doctor (me) stretched to four hours, at which point people started a light riot.
The urgent care where I was working normally has two providers at once: an MD and either a nurse practitioner or a physician assistant. That day, the nurse practitioner called out sick with COVID, leaving me alone.
Continue readingYou Must Comply
Guess who graduated residency… but is still in training!?
So now I’m starting my toxicology fellowship. I’m now at a different large academic center, still on the West Coast, and am six weeks in.
Fellowship is going well, except that I wake up every day consumed with a blinding and violent rage – not toward my training program but toward the university’s HR department.
Continue readingPushing Back On Pushback
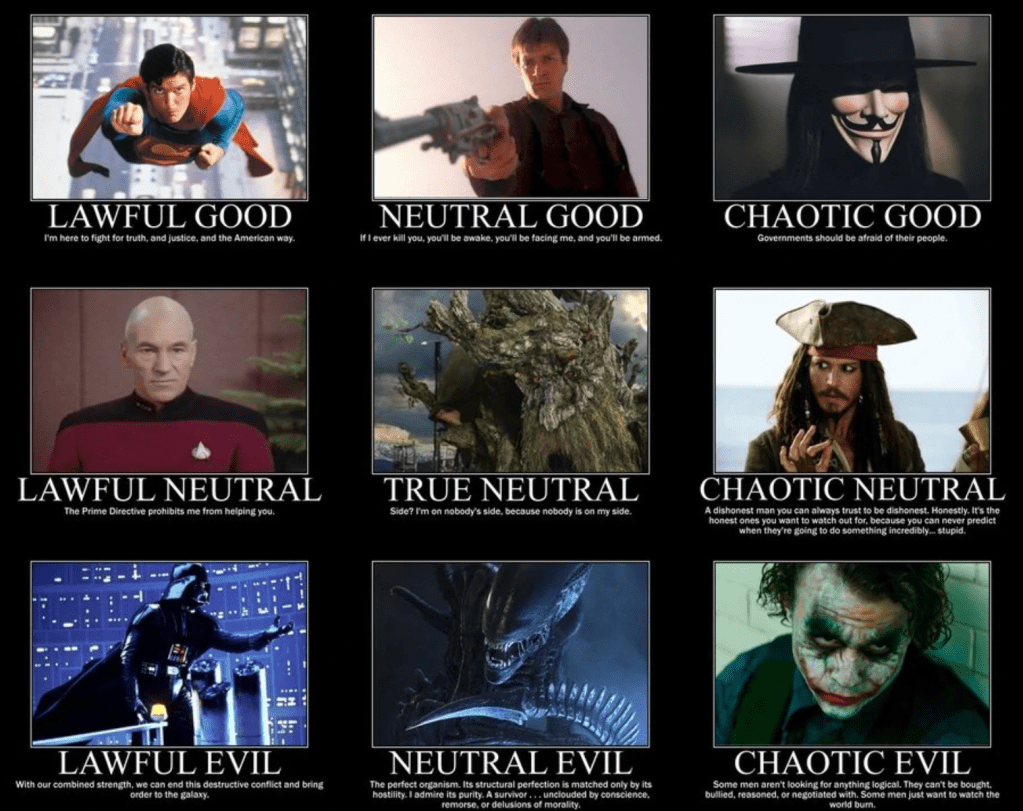
I was working on writing this gigantic 4,000-word monstrosity of a post where I tried to align specialty services with the old-school Dungeons and Dragons “Lawful/Chaotic vs Good/Evil” axes for character generation, and it was exactly as complicated as it sounds.
As I worked my way through it, I realized that half of what I wrote was about convincing specialists to come down to the ER and see my patients. At large academic centers where we residents train, we are almost always calling other residents for this task – and therein lies the rub. Like us, they are overworked and underpaid a flat salary to do their jobs. When I call the surgery resident for a consult, for example, I am creating work for them.
Continue readingAn ER Doc’s Primer On The COVID Vaccine
Hello! Once again it has been forever, but I don’t care. I’ve been too busy trying to prevent my head from exploding from, once again, people being stupid.
(I am a tiny bit frustrated with vaccine hesitancy, which I sort of understand, and very frustrated with COVID deniers and other conspiracy theorists, who I think should be first boarded onto a 13-hour Spirit Airlines flight and then forcibly ejected out the emergency exits at 35,000 feet.)
Continue readingThe COVIDpocalypse is Here and I’m Coping By Writing Again
I would like to blame my prolonged absence again on COVID-19. To be fair, it does dominate about 95% of my work life and probably 50% of my personal life, but honestly, I’ve just gotten lazy.
The last time I published here was March 5, where I started with “it seems like we are inevitably headed for a massive, global pandemic.” For once on this blog, I get to say I WAS RIGHT ABOUT SOMETHING IN RESIDENCY! No attending or dad can correct this.
As of this writing, my area’s daily hospitalization rates look like a Space-X rocket launch. We’re out of ICU beds, regular beds, gurney, cots, sleeping bags, and patience. The worst is somehow yet to come. I am coping with this impending doom by playing with my dog and, finally, writing again.
Continue readingSecond Year Is (Almost) Over
In a little more than a month, the new interns will arrive. Much like last year when I wrote “Intern Year is Over,” I greet this milestone with joy and relief – not because I am thrilled and excited for the interns to roll in, but because I am thrilled and excited to be DONE. WITH. SECOND. YEAR.

“Why?” the interested reader/grandma may ask. After all, if intern year is when you learn the byzantine system that is medicine at two different academic centers, second year is when you focus on your actual medical knowledge. Your procedural skills. Your team-based communication. Continue reading
The Residency Drowning Triad
I have not written in quite some time because I have been on a terrible rotation consisting almost entirely of things I despise: rounding, nights, and potassium.
That’s right – I’m back on a cardiac ICU unit! Continue reading
In Defense of Burnout
After an overnight shift where I spent five hours of eight on the phone transferring out three patients with brain tumors to three different hospitals because I was working at NARH, I read an article entitled, “Leading Healthcare Organizations Declare Physician Burnout As ‘Public Health Crisis.’”
(Yes, mom, I know that’s a run-on sentence.) Continue reading
Not My Hill
The journey through second year of residency is an interesting one. As I’ve mentioned before, we are tasked with two major, new responsibilities: performing most procedures and seeing a much greater volume of patients. We’ve all gone through a substantial adjustment period. It’s been hard.
One of these journeys is toward two, or greater, patients per hour. I hit this milestone rather infrequently. In fact, it is about as likely for me to achieve this as I am to win a game of Oregon Trail. It is far more likely that I will die of dysentery, or make it no further than Fort Collins before my oxen quit on me. Continue reading